Dear Covenant community,
As the COVID-19 pandemic has spread with almost unimaginable speed around the world, social media and the news have been filled with a raft of opinions, partial information, and misinformation.
It’s difficult to know who to believe, especially because subject-matter experts have confessed uncertainty about how many important aspects of the pandemic will develop. It is particularly difficult to know what will happen next because this is an entirely new sort of international crisis: while much worse pandemics have swept through human populations in the past, none of them occurred in the age of rapid international travel, instant communication, and widespread economic globalization.
Nonetheless, there is a great deal of important information that we do know now. Spreading information from reliable sources can calm fear, point to productive next steps, and contextualize this crisis in time and place.
In this article, we’ve assembled a “FAQ” of sorts, in which we have used the latest information from CDC, WHO, ECDC, the New York Times, Johns Hopkins University, NEJM, and a limited number of preprint articles. We hope that this will prove a helpful resource as we all learn more about this unusual situation.
You are always in our thoughts and prayers,
Davy Codington
Class of 2021, Biology (Biomedical)
Will Payne
Class of 2020, Biology (Environmental) and Community Development
What is COVID-19?
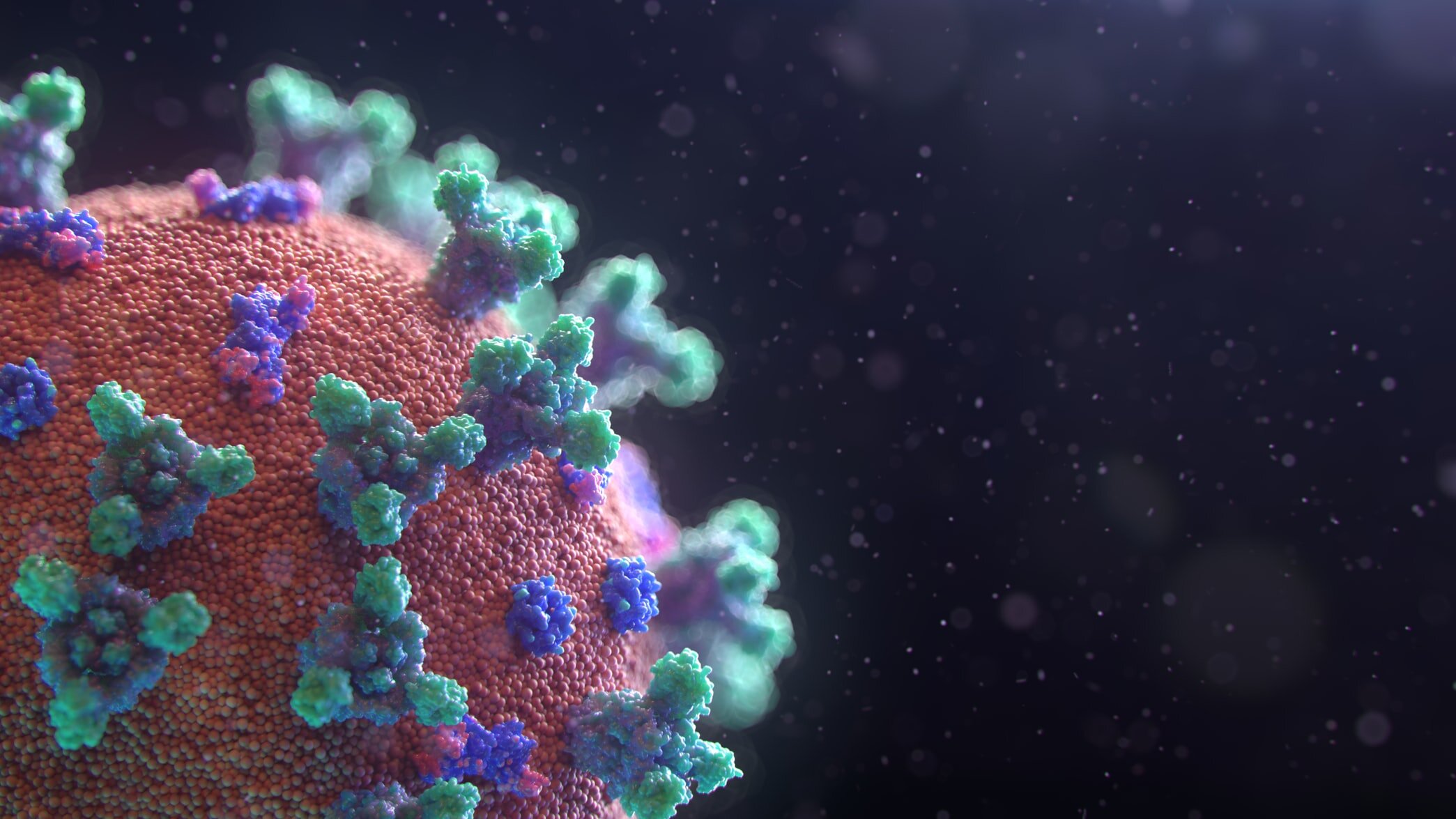
COVID-19 is the disease caused by the virus SARS-CoV-2, which is a coronavirus, a member of a group of viruses that cause respiratory illness in humans and can spread between animals and humans. The first cases were reported in Wuhan, China, in December 2019, making SARS-CoV-2 a “novel,” or new, coronavirus. Two other well-known coronavirus outbreaks are the MERS-CoV outbreak in Saudi Arabia in 2012, reaching 27 countries and infecting roughly 2500 people with a mortality rate of 34%, and the SARS-CoV outbreak from 2002 to 2004 that reached 30 countries, infecting roughly 10,000 people with a mortality rate of 9.6%. Like MERS and SARS, the symptoms of COVID-19 include fever, a dry cough, and shortness of breath. Symptoms range from mild--such as a cough--to severe, including respiratory failure.
The virus spreads through respiratory droplets carrying viral particles. A study published on March 17 in the New England Journal of Medicine reports that viral particles can persist on surfaces such as doorknobs and cellphones for up to two or three days. Respiratory particles are constantly expelled when you breathe through your nose and mouth but especially when you cough and sneeze, and can persist in the air for up to 30 minutes.
The current spread of COVID-19 has reached well over half a million confirmed cases worldwide, and appears set to reach more than a million cases in very short order. The outbreak has moved more quickly than many governments have been able to respond, and major outbreaks outside of China have occured in the United States, Italy, Spain, Iran, and elsewhere. As this article goes to press, the United States has more COVID-19 cases than any other country, and also has the fastest-growing number of deaths of any country with a major outbreak. This article details a number of the epidemiological, etiological, and clinical characteristics of COVID-19/SARS-CoV-2, and provides information about how you can protect yourself and others.
How did this pandemic start?
COVID-19 is a zoonotic disease. This means that, unlike diseases which have been spreading through human populations for a long time, this virus jumped from a single animal to a single human being at the start of the outbreak. This type of jump is not uncommon, and has occurred previously with Ebola, SARS, MERS, HIV, the 1918 Spanish influenza, and the 2009 swine influenza, among many other cases.
To the best of our knowledge, sometime in November 2019, a person in southern China consumed an exotic animal (possibly a pangolin) which had been infected with SARS-CoV-2 through contact with a bat. Many dozens of coronaviruses have their natural reservoir in bats, and it is very likely that the first human infected with SARS-CoV-2 contracted a bat coronavirus through an intermediate carrier animal. This is the same pathway that SARS-CoV took 18 years ago, when it jumped from a bat, to a civet (a vaguely cat-like nocturnal mammal), to a human. The genome of SARS-CoV-2 is 96% identical to a known bat coronavirus, and bears limited genetic evidence that it passed through pangolins at some time in the past.
The large coronavirus reservoir in bats was called a “time bomb” by scientists investigating the SARS-CoV outbreak in 2002. Many ecologists studying zoonoses believe that jumping events like this one are becoming increasingly common as humans expand logging and agricultural activities further into undisturbed natural areas.
We spoke to Dr. Heath Garris, an ecologist on faculty at Covenant College, who said, “The high percentage of recent emerging diseases coming from animal sources (~75%) is alarming… Ecologists have speculated that a rise in spillover events (and ensuing epidemics) is one consequence of increasing proximity between humanity and wildlife, especially in areas that combine high population densities of people and likely reservoir hosts (mammals like bats, rodents, or primates).”
Why is COVID-19 a dangerous disease?
Some accounts have emphasized the fact that COVID-19 is a mild illness for most people. On the contrary, this is one reason why COVID-19 is so dangerous, and why it has spread so quickly. While 80% of cases are so mild that individuals may not take their illness seriously, 20% of cases are so severe that highly specialized (and scarce) hospital treatment may be necessary.
When a young person in otherwise good health contracts COVID-19, probabilities are good that they will experience a dry cough, unusual tiredness, a fever, a sore throat, and rarely severe symptoms such as difficulty breathing. Modeling studies suggest that a large proportion of infections (from 48% to 62%, according to the European CDC) are caught from someone else who has not yet started showing symptoms, and a large percentage of the remaining cases are caught from someone else who is only showing mild symptoms.
When a person develops severe illness, they are likely to experience extreme shortness of breath, which may eventually develop into a severe pneumonia. It is these patients who will require the critically important machines that have been the subject of so much recent discussion: ventilators.
When a patient becomes unable to breathe for themselves, due to an injury or infection, or during surgery, doctors can place a tube into their windpipe to artificially inflate their lungs. The machines that do this are highly specialized, and the United States has only about 200,000 of them, many of which are already in use on any normal day. Shockingly, as many as 900,000 COVID-19 patients may require ventilation in the United States before the end of the pandemic, according to the Society of Critical Care Providers. If all of these cases occur at once, there will be no way to care for all the patients who need advanced care. If cases can be spread out over time, however, many more patients can receive the ventilation they need to stay alive.
This is why COVID-19 is so dangerous: it spreads easily and pre-symptomatically, and it is severe enough in a large enough percentage of people to overwhelm critically under-resourced health systems.
How does COVID-19 compare to other diseases?
There have been many reports in the news and on social media that COVID-19 is “just a bad flu.” It is fundamentally not. These reports tend to obscure the true risks of COVID-19 and prevent reliable comparison between COVID-19 and other diseases.
At this time, it appears that COVID-19 has a very much higher mortality rate, and a faster rate of spread, than the seasonal flu and the 2009 swine flu pandemic.. At the same time, it is probably not as severe as SARS, the 1918 Spanish Flu, or smallpox.
The important number to understand when we talk about how infectious a disease might be is called “R0” (pronounced “R-naught” or “R-sub-zero”). R0 is the average of how many new infections a single patient with a disease is likely to cause in one generation. For the seasonal flu, this number is between 1 and 3 (median 1.3), meaning that one patient will create, very approximately, 14 additional infections over 10 generations. For COVID-19, this number appears to be between 1.5 and 3.5 (median 2.8), meaning that one patient will create, very approximately, 29,600 additional infections over 10 generations. Add to this the fact that the seasonal flu has about a 0.1% fatality rate, while some countries seem to have experienced a fatality rate as high as 4% for COVID-19, and the true potential severity of this disease begins to emerge.
This chart prepared by the New York Times highlights the differences in virulence and mortality between COVID-19 and other common diseases:
What are key metrics for understanding the speed and scope of the pandemic?
There is a great deal of uncertainty about when the pandemic will slow down, and how much damage it will cause before it does. Several key statistics, however, can provide early signs that an epidemic is beginning to slow in a particular region:
Doubling time of SARS-CoV-2-related deaths: No country currently has enough testing capacity to know about every person who is sick, but many countries can accurately track the number of patients who have died of the virus. As this article is being written, deaths in the United States are doubling every two days, while deaths in South Korea are doubling every two weeks--in real terms, this means that the South Korean outbreak is relatively contained, while the U.S. outbreak is not. Look for increased doubling time as a good sign that the outbreak is beginning to slow. We recommend this NYT tracking site for keeping up with this metric: https://www.nytimes.com/interactive/2020/03/21/upshot/coronavirus-deaths-by-country.html
New COVID-19 cases reported per day: If an epidemic is still growing exponentially, there will be an increasing number of new cases every day. If it is slowing, new cases per day will be about the same as the previous day, or lower. While this metric has the disadvantage of relying on often-spotty testing, it has the advantage of being closer to “real-time,” and excludes effects related to health system preparedness. We recommend this Johns Hopkins University tracker for viewing daily cases (click on “Daily Increase” in the lower right hand corner): https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
What is “flattening the curve”?
“Flattening the curve” has become the mantra of the global effort to slow the spread of COVID-19. “The curve” refers to a bell curve plot of the number of infected people in an epidemic across time. When the curve is steep, a large number of cases has occurred in a relatively short period of time. When the curve is broad and “flat,” the caseload of the infectious agent is spread across time. The phrase “flattening the curve” is used by epidemiologists to state in shorthand that if an infectious agent cannot be stopped immediately, the goal is to spread the caseload through time. This makes the burden of disease more manageable for health systems and governments.
The health system in the US is designed to function at nearly full capacity almost all of the time. Unfortunately, this means that a rapid outbreak of COVID-19 can result in an influx of patients with serious respiratory illness that hospitals are not designed to handle all at once.
When sick people are able to access the health system to get the care they need, irreversible damage by the virus is avoided. When the health system is receiving more patients than it can take on at a given time, the patients that it cannot take on will suffer. Flattening the curve through social distancing and proper hygiene distributes the patient load through time so that health systems are able to deliver appropriate care to each patient. As patients recover from infection, new patients will be able to more readily access the system, increasing their chances of survival and decreasing the overall number of deaths from COVID-19.
Why has the U.S. struggled to control its COVID-19 outbreak?
Both China and South Korea have seemingly contained their COVID-19 outbreaks, at least for the time being. Both countries have relatively low growth rates of new infections and new deaths. How did they do it, and why is the United States struggling to follow suit?
China appears to have stopped the virus on the basis of two extreme measures: complete police-enforced lockdown of millions of people, and rapid, widespread testing of every person believed to have the virus. Lockdown measures, while possibly successful, are legally and socially unfeasible in a Western economy.
Fortunately, South Korea, which has an open economy more similar to the United States, managed to halt the virus without resorting to martial law. It did so by relying on rapid testing alone, which it has implemented more quickly and effectively than any other country.
Following its 2015 MERS outbreak, South Korea’s health officials realized that strategic stockpiles of testing supplies were needed to halt future fast-moving disease outbreaks. Because of this, they developed stockpiles of PCR reagents--the chemicals needed to detect the genome of a disease in a sample--and developed logistics plans to deploy testing sites around the country. As soon as COVID-19 appeared, South Korea invested in the production of testing kits and created a large number of drive-through testing sites, where patients could approach a site in their vehicle and be tested, without leaving their car. By deploying a very large number of tests, along with rigorous “contact tracing” of all the people who could have been exposed, South Korea seemingly managed to detect and isolate many presymptomatic cases and slow down transmission considerably.
In the United States, federal and state governments were unprepared to secure supplies of testing reagents, of which there is now a national shortage, and key missteps by the CDC in the first weeks of the outbreak prevented testing kits from becoming widely available until after the virus had already escaped any attempts at containment. The country is now forced onto its back foot, only having the resources to test high-risk patients as cases continue to increase. While this will help diagnostic decisions in difficult cases, it is insufficient to identify every case, and most patients will not know that they need to self-isolate. This shortage means that “social distancing” is the only measure which will be able to slow the spread of the virus in the near term.
How bad is it going to get? How long will it last?
No one is sure how bad the pandemic will become, because it is a virtually unprecedented event. Reporting by FiveThirtyEight and The Atlantic, in which interviews of groups of epidemiologists were used to generate worst case, best case, and median scenarios, have revealed roughly three groups of predictions:
The epidemic will spike in the next one to two months, killing many people, but creating vastly expanded herd immunity once everyone recovers. This is the worst-case “doomsday” scenario in which mitigation efforts virtually fail. While it is the fastest route to recovery, it is also the most harmful, as a large spike in cases would quickly overwhelm the health system. Hospitals, governments, and public health authorities need time to scale up testing, ventilator production, and supplies of masks and other protective equipment. This scenario would not give them enough time.
We find effective treatments, massively scale up testing, or discover that the virus is somewhat seasonal in the next three to five months, allowing for a slow return to normal. This scenario is more likely, but it requires an enormous amount of work, and a great deal of luck. It is hoped that some hidden factor we don’t know about yet (a seasonal pattern in transmission, a drug which lets us keep more patients off ventilators, a national testing and contact-tracing program with extremely high effectiveness) would allow us to relax certain measures, such as reopening restaurants, offices, and schools. It is unlikely, however, that social distancing measures will be entirely abandoned for at least a year. Events with large crowds, for instance, are unlikely to occur again for quite some time, and continued high levels of hand hygiene will be extremely important.
Our mitigation efforts become no more successful than they are now, and we must wait twelve to eighteen months for a vaccine. This is a somewhat likely scenario, especially given how woefully unprepared many governments appear to be at present. If there is no respite from an effective treatment or improved testing program, extreme social distancing measures will be necessary until a vaccine can provide everyone with immunity. The earliest timeline for small batches of vaccine production is the fall of 2020, when healthcare workers may be provided with initial doses. Vaccines are unlikely to be widely available to the general public until the spring of 2021, which (it is hoped) will put a permanent end to COVID-19.
How are we going to stop this disease?
There is only one way to permanently stop a disease from spreading: making enough people immune. There are two ways to do this: either we could allow the disease to infect 80% - 90% of the population, or we could vaccinate everyone. As detailed in the previous answer, a rapid spike in infections would result in an extreme number of deaths, while a vaccine is still many months away.
For the time being, therefore, we are stuck with mitigation strategies--using social distancing and widespread testing to reduce the number of people newly infected each day, slowing down and spreading out the wave of the epidemic.
What are good sources of information about COVID-19/SARS-CoV-2?
The most reliable information about how to protect yourself and others comes from the United States Centers for Disease Control, at www.cdc.gov. The best source for statistics on how the disease is spreading can be found on the Johns Hopkins University website at coronavirus.jhu.edu/map. For updates on the global response, see the World Health Organization at www.who.int/emergencies/diseases/novel-coronavirus-2019.
For news on the latest developments, remember to check a variety of reliable sources. We’ve tended to lean towards reading the New York Times, especially because their reporters are running several very detailed tracking projects for cases in the United States and elsewhere (see www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html and www.nytimes.com/interactive/2020/03/21/upshot/coronavirus-deaths-by-country.html). Nonetheless, reading multiple sources is essential. Check extraordinary claims against the data available from the CDC and WHO, and be slow to spread possible misinformation. Be wary of popular sources with overt political bias, such as Fox News, Daily Kos, and Infowars.
Who is at highest risk from COVID-19?
Most people are at roughly the same risk of contracting COVID-19 if they are exposed. However, once a person is infected, some people may be at much higher risk for developing severe disease (including pneumonia requiring artificial ventilation) than others. The CDC defines those at highest risk as being:
Those aged 65 and older
People who live in a nursing home or long-term care facility
People with chronic lung disease or moderate to severe asthma
People who have a serious heart condition
People who are immunocompromised (including due to cancer chemotherapy)
People of any age with severe obesity (BMI > 40)
People of any age with diabetes, renal failure, or liver failure, particularly if not well controlled
People who fall into any of these risk categories should practice special cautions beyond those recommended for everyone, including finding someone else to do their grocery shopping and errands, avoiding close contact with anyone outside their own household, and practicing excellent hand hygiene.
What about those with low income in the U.S., and people in countries with less-prepared health systems?
This virus is very new, and its initial pattern of spread has taken it through many wealthy countries, rather than to the majority world. However, there is nothing to suggest that outbreaks in the majority world will be any less severe--rather, on the contrary, all early evidence points to the notion that people who are economically vulnerable are at substantially higher risk from the virus.
Particularly in the United States, where many hourly workers have no guaranteed sick leave and millions do not have access to health insurance, it is likely that the poor will be most severely impacted. Evidence that this is occurring is already appearing in American cities like Dallas, Texas, where almost all COVID-19 testing has occurred in the wealthiest ZIP codes surrounding the city. Without access to primary care, health insurance, or reliable hospitals, individuals living in poverty or homelessness are less likely to receive care, more likely to develop severe disease due to preexisting conditions like asthma, and more likely to spread the virus due to the impossibility of social distancing in many low-wage jobs.
Internationally, many countries in Africa and some parts of South America do not have adequate reference laboratories, the advanced facilities where testing for COVID-19 must occur. If reference facilities do exist, they are almost always located in capital cities, leaving the rural poor to fend for themselves against an invisible enemy. As with almost every other infectious disease, it will eventually be the poorest citizens of the poorest nations who pay the highest cost--with this characteristic pattern likely developing as soon as this summer. It will be imperative for the global community to support health systems in the majority world during this crisis, bolstering national leadership, offering protective equipment and testing supplies, and making sure that the eventual distribution of a vaccine is globally equitable. These steps are essential both for the sake of justice, and to protect all countries from recurring outbreaks of COVID-19.
How can I protect myself? What should I do if I’m sick?
The CDC recommends, as much as feasible, minimizing your chances of being exposed to the virus. This means that you should not be in contact with people who are sick and that you should practice “social distancing,” with at least six feet between you and anyone outside your immediate household at all times. You should further protect yourself by washing yours hands often and thoroughly with soap and water. (The World Health Organization has published a hand-washing guide for thorough hand hygiene: https://www.who.int/gpsc/clean_hands_protection/en/.) It is especially important to wash your hands after being with other people, after sneezing or coughing, after blowing your nose, after using the restroom, and before and after preparing food. You should avoid touching your eyes, nose, or mouth (the sites of ingress for SARS-CoV-2) unless your hands are washed.
Notably, the CDC and WHO both strongly recommend that healthy people do not wear masks, unless they are providing care for a sick person. While masks can provide a small amount of protection for a healthy person, they are most needed by healthcare workers, and there is currently a global shortage of masks which is preventing hospitals and primary care offices from getting adequate supplies.
If you are sick (even if you only have mild symptoms!), it is important to avoid contact with others who have not been sick with the virus, unless otherwise directed by your medical provider. Self-quarantine is imperative to prevent spread of the virus. Other essential practices from the CDC if you are sick: cover mouth and nose when coughing or sneezing, wear a mask when around others, and disinfect surfaces you come into contact with using alcohol or bleach solutions. If you are sick, ask your medical provider for guidance on when you are able to stop self-quarantine.
Am I protected if I have recovered from being sick with the virus?
In part, yes. However, there is more to the story. While contracting a viral infection and recovering does produce antibodies--defense molecules that make one “immune” to the viral agent--these antibodies may have a limited lifespan within your body. While some infections produce antibodies that last a lifetime (on the order of 40+ years), some infections produce antibodies that last just months. We do not yet understand how immunity to COVID-19 works.
It is possible that children can attain immunity without showing symptoms. Further, it is possible that multiple strains of COVID-19 will develop, just as multiple strains of influenza have developed, which would make antibodies to a particular strain less useful. These questions remain unanswered. The CDC states that it is not yet known whether exposure and recovery will lend immunity to COVID-19. Regardless of the possibilities, the best thing to do is to maintain social distancing and avoid contact with those who have been exposed to the virus.
The Journal of Clinical Investigation has explored the possibility of treatment using human convalescent serum (https://www.jci.org/articles/view/138003). Convalescent serum is a dose of antibody from someone who has recovered, administered to someone else. A brief report from China suggests that small-scale treatment (and possibly prevention) with convalescent serum is effective and feasible (http://www.xinhuanet.com/english/2020-02/28/c_138828177.htm).